When BQK was only 5 years old, the first seizures came like fierce waves, without warning. Ms. CLV's family ( Hanoi ) rushed to take their child everywhere for help. Every hospital had the same diagnosis: the child had epilepsy.
The frequency of seizures is increasingly dense, sometimes up to dozens of times a day, lasting for many consecutive days. Prolonged seizures not only put the child at risk of falling and injury, but also seriously affect physical and intellectual development.

By 2024, K. showed signs of drug resistance – a condition that experts call refractory epilepsy . Despite using the maximum dose and a combination of drugs, the seizures continued to strike as if the child’s body rejected all attempts at treatment.
“At first, my child responded well to the medication, but by 2024, his illness had worsened and he began to show signs of drug resistance. Despite increasing the dose and combining many different medications, the seizures still could not be controlled,” Ms. V. shared.
Faced with that situation, Ms. V. decided to take her child to Ho Chi Minh City, to Vinmec Central Park International General Hospital - the place where there was the last bit of hope left.
MSc. Dr. Tran Thi Phuoc Yen, Neurologist, Department of Examination and Internal Medicine, Vinmec Central Park International General Hospital (HCMC), said that resistant epilepsy is a condition in which epileptic patients do not respond to drug treatment even though the maximum dose has been increased and many different antiepileptic drugs have been combined. Patients with resistant epilepsy are often at high risk of complications due to prolonged seizures.

In cases of resistant epilepsy, surgical removal of the epileptic focus is considered one of the optimal options. According to world medical literature, epilepsy surgery helps 60-80% of patients to be free of epilepsy after surgery. However, according to Dr. Yen, accurately determining the epileptic focus in the brain is also a major challenge for doctors when the lesion is large, deep and difficult to identify with conventional assessment techniques.
The case of baby K. is a typical example. When arriving at Vinmec Central Park International General Hospital (HCMC), the patient was identified as a difficult case because the child was diagnosed with epilepsy very early (5 years old), with prolonged and frequent seizures.
“At the time of admission, the child was 9 years old and was taking many anti-epileptic drugs at maximum doses but still could not control the seizures. This significantly affected the child’s quality of life as well as his future development.
Meanwhile, conventional techniques such as scalp electroencephalography, brain MRI and PET scan cannot determine the location of the epileptic focus," Dr. Yen added.
Without finding the epileptic focus, the doctors could not operate. If they did not operate, the child would have to live a life of pain, with the potential for irreversible brain damage. The doctors were faced with an extremely difficult problem.


An important step before surgery is to accurately determine the location of the epileptic focus.
7 days before the surgery, doctors from many specialties such as Neurosurgery, Neurology, Diagnostic Imaging... continuously consulted to evaluate and delineate the brain area with the potential for epileptic focus before placing electrodes intracranial.
This is the first time the intracranial electrode method has been performed in Vietnam with the participation of Japanese expert, Associate Professor Nakae Shunsuke. This greatly supports the timing of the procedure as well as the surgical process of removing the patient's epileptic focus later.
In addition, this is also the first time Vietnam has applied the Autoguide Robot method to locate electrodes deep in the brain to treat resistant epilepsy, helping to accurately position the electrodes in the brain. The Autoguide Robot acts as a positioning system to accurately determine the desired location to place the electrodes in the patient's cerebral cortex at safe locations.

Dr. Yen analyzed that compared to traditional positioning methods, Robot Autoguide helps to accurately determine the target for electrode placement. The electrode placement speed will be faster because the number of electrodes needed to be placed is very large - up to 6 positions, helping to shorten the surgery time. The pre-programmed robotic arm will help to place the electrode in the desired position, minimally invasive, without causing damage to brain tissue, avoiding affecting the baby's neurological function later.
The process of placing intracranial electrodes requires careful calculation to be able to insert the electrodes without rupturing blood vessels, avoiding complications of intracranial hemorrhage, so the programming is time-consuming and elaborate. The surgeon also needs to know how to use the robotic arm to choose the appropriate approach.
Intracranial electrodes are connected to the Arc Zenith multi-channel EEG system, allowing support in identifying epileptic foci, language, motor, and sensory areas – helping to avoid damage to these functions during surgery to remove epileptic foci.

The surgery to place the intracranial electrode in the child took about 5 hours and after 7 days, the doctors had determined the exact location of the epileptic focus. However, the difficulty did not stop there, the surgical removal was also a real challenge for the doctors.
Master, Doctor Truong Van Tri, Head of Neurosurgery Department, General Surgery Department, Vinmec Central Park International General Hospital, and his team performed surgery to remove the area of the brain with this epileptic focus. The surgery lasted about 5 hours.
“Because the patient is still young, the surgery needs to be performed quickly to minimize the risk of blood loss and infection.
In addition, the epileptic focus was determined to be located in the right orbital region and the right inferior frontal lobe, so the surgeon must operate skillfully and precisely to avoid damaging large blood vessels and important nerve structures in this area such as the patient's olfactory nerve and optic nerve," said Dr. Tri.
After surgery, the child recovered well and was closely monitored by many different specialists. Witnessing the child's recovery day by day, the doctors could not help but be moved.

After more than 1 month of surgery, baby BQK recovered well, living and playing normally, without any neurological defects. Only 2 mild seizures were recorded during sleep - compared to dozens of seizures per day before.
The doctors could not hide their emotions when they saw K. smile on the day he was discharged from the hospital. “We have seen him tired for a long time. Now he can go to school, integrate with his friends, and his bright future is open again,” Dr. Yen said emotionally.
The young mother, who once thought she would never recover from her child’s illness, is now able to see her child sleep soundly. “Now I can have a normal dream – to see my child grow up every day like any other child,” Ms. V. said emotionally.
“There are many patients with resistant epilepsy, but we cannot accurately determine the epileptic focus using conventional methods such as scalp electroencephalography, brain MRI and PET scan, which have been used in Vietnam for a long time. Therefore, patients have to live with the epileptic seizures that torment them every day,” Dr. Yen shared.
However, with the development of modern medicine, the technique of placing intracranial electrodes with robot support has opened a new turning point in the treatment of the disease. This technique allows doctors to accurately identify the epileptic focus, especially the focus deep in the brain, which is difficult to do with traditional methods. Thanks to that, many patients have the opportunity to completely remove the epileptic focus, thereby escaping this terrible disease.
For children, successful treatment is even more meaningful. It not only helps to cure the disease but also saves the future. A child who is treated in time will no longer have to bear the burden of psychology, learning, social development, even intelligence, all can be saved.

Determining where to place the electrodes is a very important factor. Each electrode represents a large cost, so the number of electrodes and their placement should be optimized. The more electrodes placed, the more expensive the treatment, the longer the surgery, and the higher the risk of infection.
Dr. Tri also expressed his hope that the use of robotic arms will become a routine service in epilepsy and brain tumor surgeries.
“The effective coordination between the Neurology & Neurosurgery, Diagnostic Imaging, Pediatrics, and Anesthesia teams in accurately determining the location of the seizure as well as performing electrode placement and surgical removal of the epileptic focus helped the surgery to be a success. In Ho Chi Minh City, very few units specializing in epilepsy can do this,” said Dr. Tri.
Vinmec is aiming to standardize the use of Autoguide robots as a routine treatment procedure for complex epilepsy cases, opening up great hope for the patient community.
From a seemingly hopeless disease, a miraculous journey was written. And on that journey, medicine was the guiding light that brought a child back to the normal world, with a smile and a complete childhood.
Source: https://dantri.com.vn/suc-khoe/cau-be-9-tuoi-va-hanh-trinh-vuot-con-ac-mong-mang-ten-dong-kinh-khang-tri-20250728114008016.htm



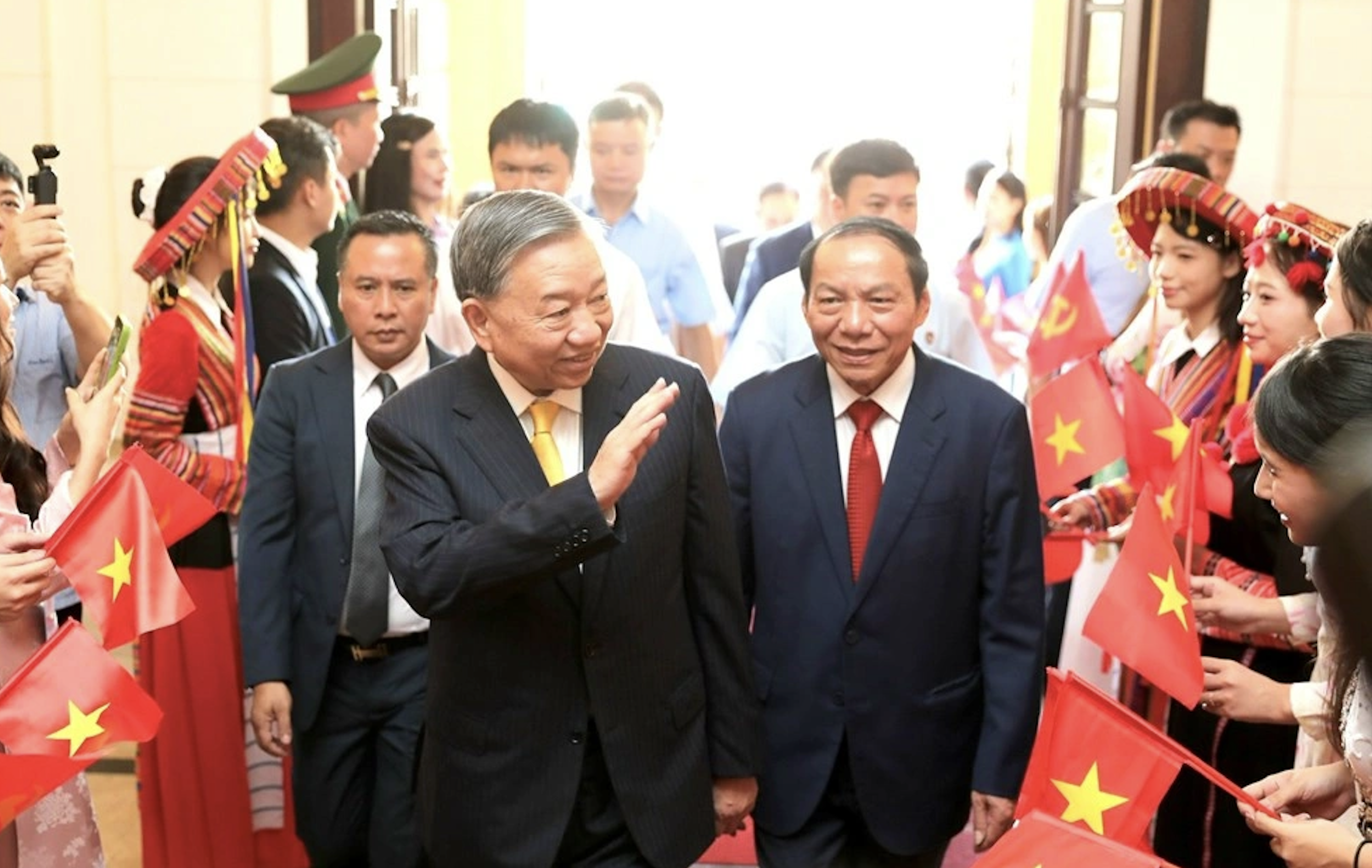
![[Photo] General Secretary To Lam attends the 80th Anniversary of the Cultural Sector's Traditional Day](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/8/23/7a88e6b58502490aa153adf8f0eec2b2)



























































































Comment (0)